 Snapping
scapula syndrome, or otherwise known as scapulothoracic crepitus, is
a disorder in which scapulothoracic motion produces a snapping,
grinding, thumping or popping sensation (1, 2). The sound is produced
by a tactile-acoustic phenomenon of which there exist a multitude of
potential causes ranging from bone spurs to muscular weakness to
bursitis (2). While most patients experience “snapping scapula” as
merely an annoying, asymptomatic crepitus, some do report a direct
correlation between the sound and the onset of pain, which can
result in a truly disabling condition (1).
Snapping
scapula syndrome, or otherwise known as scapulothoracic crepitus, is
a disorder in which scapulothoracic motion produces a snapping,
grinding, thumping or popping sensation (1, 2). The sound is produced
by a tactile-acoustic phenomenon of which there exist a multitude of
potential causes ranging from bone spurs to muscular weakness to
bursitis (2). While most patients experience “snapping scapula” as
merely an annoying, asymptomatic crepitus, some do report a direct
correlation between the sound and the onset of pain, which can
result in a truly disabling condition (1).
 It is important to note that the scapulothoracic joint is not a true
synovial joint, yet merely an articulation between the anterior
scapula and the posterior thoracic cage with no attachment by
fibrous, synovial or cartilaginous tissue (3). This pseudo-joint
between the scapula and the thoracic cage is the most incongruent
articulation in the body, yet plays a crucial role in upper
extremity function and provides a stable base for glenohumeral
motion. This simultaneous, coordinated movement between the
scapulothoracic and glenohumeral joint produces what is known as
“scapulohumeral rhythm”, which consists of a motion ratio of 2° of
glenohumeral elevation to every 1° of scapulothoracic elevation.
Movement occurs along the plane of the scapula, which axes lie
30°-40° in frontal plane and 10°-20° anterior from vertical plane
(4).
Scapular function is mostly maintained through dynamic muscular
control of the following surrounding musculature: pectoralis minor,
coracobrachialis, serratus anterior, triceps, biceps, subscapularis,
rhomboids, levator scapulae, trapezius, deltoid, supraspinatus,
infraspinatus, teres minor, teres major, latissimus dorsi and
omohyoid (5).
It is important to note that the scapulothoracic joint is not a true
synovial joint, yet merely an articulation between the anterior
scapula and the posterior thoracic cage with no attachment by
fibrous, synovial or cartilaginous tissue (3). This pseudo-joint
between the scapula and the thoracic cage is the most incongruent
articulation in the body, yet plays a crucial role in upper
extremity function and provides a stable base for glenohumeral
motion. This simultaneous, coordinated movement between the
scapulothoracic and glenohumeral joint produces what is known as
“scapulohumeral rhythm”, which consists of a motion ratio of 2° of
glenohumeral elevation to every 1° of scapulothoracic elevation.
Movement occurs along the plane of the scapula, which axes lie
30°-40° in frontal plane and 10°-20° anterior from vertical plane
(4).
Scapular function is mostly maintained through dynamic muscular
control of the following surrounding musculature: pectoralis minor,
coracobrachialis, serratus anterior, triceps, biceps, subscapularis,
rhomboids, levator scapulae, trapezius, deltoid, supraspinatus,
infraspinatus, teres minor, teres major, latissimus dorsi and
omohyoid (5).
ETIOLOGY
Snapping scapula syndrome is thought to be caused by irregular
motion between the scapula and thoracic ribcage (2-3, 6). This abnormal scapulothoracic motion can be the result from one of several
causes (7-9):
| Bony Prominences |
¨
Luschka tubercle*
¨
Abnormal curvature of scapular superior angle
¨
Curling of vertebral border
¨
Irregularities of subscapular ribs
¨
Exostosis of subscapular ribs |
| Tumors |
¨
Osteogenic
sarcoma
¨ Osteochondroma
¨ Chondrosarcoma |
| Structural Spinal Abnormalities |
¨
Scoliosis
¨ Thoracic
kyphosis |
| Fracture |
¨
Fracture
malunion of ribs or scapula
(causing bony angulation and/or increased callus
formation) |
| Dyskinesis: Loss of Dynamic Control |
¨
Muscle overuse
¨
Muscle imbalance (often following nerve injury)
¨
Muscle atrophy (following nerve injury, trauma or
prior operative treatment)
¨
Common in patients with
shoulder instability, impingement and rotator cuff
abnormalities |
| SICK
Scapula |
Overuse Muscle
Fatigue Syndrome:
¨
Scapular
Malposition
¨
Inferior
Medial Border Prominence
¨
Coracoid pain and malposition
¨
Dyskinesis
of scapular movement |
* Hook-shaped prominence at superomedial
angle of scapula
EXAMINATION
Performing a thorough examination is vitally important to creating
an appropriate treatment plan for individuals with snapping scapula
syndrome. Below are some essential components to the subjective and
objective examination of individuals who present with snapping
scapula syndrome:
Subjective Exam (10):
| |
Symptomology: |
| |
- Duration, frequency, severity, location of symptoms |
| |
- MOI (mechanism of injury): insidious onset, with change in
activity
..pattern, or associated with trauma |
| |
- Associated symptoms: shoulder girdle and/or neck pain; weakness |
| |
Psychosocial: |
| |
- Occupation, activity level, hand dominance |
|
Objective Exam (1, 7, 9):
| |
1. Postural conditions: thoracic kyphosis, forward-tilted
head, rounded
|
....shoulders, abducted/forward-tipped scapulae, suboccipital
...
extension |
|
| |
2. Referred pain: cervical radiculopathy, neurological
injuries |
| |
3. Scapular asymmetry: scapular position in protraction
versus
... retraction versus rotation; compensations with trunk shifting
....(observe with wall push-up) |
| |
4. Palpation: focal tenderness of medial scapular border over
... superomedial and/or inferomedial bursae (patient position: adduct
....and internally rotate shoulder while touching opposite scapula) |
| |
5. Static Strength: trapezius, rhomboids, levator scapulae,
serratus ...anterior, latissimus dorsi, rotator cuff muscles, deltoids |
| |
6. Dynamic strength: Presence of scapular winging: lateral
winging
...(injury to long thoracic nerve that results in serratus
anterior
... atrophy);
shoulder drooping and forward rotation
(injury to
spinal
....accessory nerve that results in trapezius atrophy) |
| |
7. Muscle flexibility: Hypertonia, myofascial tightness
(common in
...upper trapezius and pectoralis minor), posterior capsular
....tightness; from chronic overuse or postures that hold muscles in
....shortened positions |
TREATMENT
For the most part, scapulothoracic crepitus can be managed
nonoperatively via treatment options such as physical therapy,
anti-inflammatory medications, and corticosteroid injections (7, 12-14).
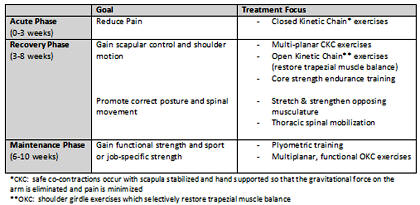
Physical Therapy. Goals of rehabilitation center on
addressing postural issues, improving muscular strength, endurance
and balance, and working on core strength. Kibler and McMullen (15)
introduced the concept of a kinetic chain system that is built from
the premise that efficient shoulder motion and muscle activation
occur in a proximal-to-distal sequence, wherein shoulder function
(distal) is dependent on thoracic spinal control (proximal). They
centered their ten week shoulder rehabilitation program on the
kinetic chain system and identified three stages of rehabilitation:
acute, recovery and maintenance phases (15).
Click here to
see enlarged table.
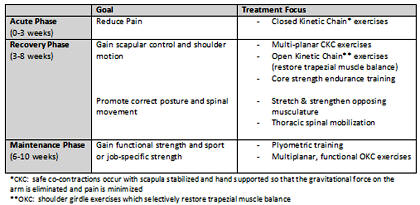
The following are several key points to
consider during the rehabilitation of snapping scapula (15-17):
| |
- Recognize and correct compensatory motions. Often from
scapular
..muscular fatigue; key into trunk shifting with arm activity
and correct
..via appropriate strengthening and postural awareness |
| |
- Emphasize endurance training. Low intensity, high volume
exercise for more functional training stimulus. |
| |
- Utilize force couple with overhead movement. Co-contraction
of serratus anterior and upper/lower trapezius in opposite
directions to
produce upward rotation of scapula. |
| |
- Focus on proper, appropriate exercise progression.
Isometric → isotonic → eccentrics; closed kinetic chain → open
kinetic chain; for
maximal restoration of functional strength |
| |
- Address common associated issues/abnormalities: biceps
tendinitis, thoracic outlet syndrome, rotator cuff pathology, and
even
headaches |
Injections. Injections can be used diagnostically and
therapeutically. Corticosteroid or local anesthetic can be injected
into the scapulothoracic bursa for pain relief anywhere from six
hours to fifteen months (17). While overall fairly safe, one
potentially fatal complication of injections in this area is that of
a pneumothorax (7). Recent technology is revealing the use of
ultrasound-guided injections for increased accuracy of injections;
however, clinical evidence for its efficacy has yet to be determined
(18).
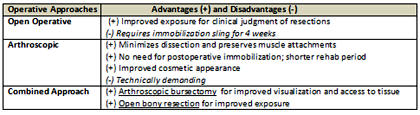
Operative Treatment. When all conservative resources have
been exhausted, operative treatment should be considered for
resection of osseous abnormalities and/or removal of inflamed bursae.
Predictors of poor operative outcome include failure to receive
temporary relief from injection therapy, inability to voluntarily
reproduce snapping scapular sound, involvement in Workers’
Compensation claim or litigation, and documented nerve deficits (7).
Three surgical approaches are open operative, arthroscopic and
combined (19-20).
Click here to
see enlarged table.
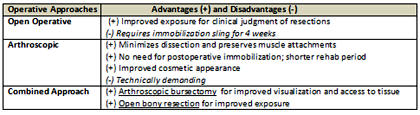
Although previous case series have often
found favorable results with operative treatment, the sample size
has been small and techniques have been inconsistent and varied.
Nonoperative treatment should continue to focus on addressing
associated impairments and following an appropriate exercise
progression through the various stages of rehabilitation. Indeed,
great importance needs to be put on continued investigation to more
specifically establish the most effective treatment strategies for
this complex, multifactorial condition.
Last revised: April 20, 2013
by Jennifer Werwie, DPT
References:
1) Milch H. Partial scapulectomy
for snapping of the scapula. J Bone Joint Surg Am. 1950;32:561-6.
2) Cuillo JV, Jones E. Subscapular bursitis: conservative and endoscopic
treatment of “snapping scapula” or “washboard syndrome”. Orthop Trans. 1993;
16:740.
3) Poppen NK, Walker PS. Normal and abnormal motion of the shoulder. J Bone
Joint Surg Am. 1976;58:195-201.
4) Voight ML, Thompson BC. The role of the scapula in rehabilitation of
shoulder injuries. J Athl Train. 2000;35:364-372.
5) Della Valle CJ, Rokito AS, Birdzell MG, Zuckerman JD. Biomechanics of the
shoulder. In: Norkin M. Frankel NH, eds. Basic Biomechanics of the
Musculoskeletal System. Philadelphia, PA: Lippincott Williams & Wilkins;
2001:318-339.
6) Milch H, Burman MS. Snapping scapula and humerus varus. Report of six
cases. Arch Surg. 1933;26:570-88.
7) Lazar MA, Kwon YW, Rokito AS. Snapping scapula syndrome. J Bone Joint
Surg Am. 2009, 91:2251-2262.
8) Rockwood CA Jr, Matsen FA III, Wirth MA, Lippitt SB. The shoulder. 3rd
ed. Philadelphia: Saunders; 2004.
9) Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder:
spectrum of pathology Part III: The SICK scapula, scapular dyskinesis, the
kinetic chain, and rehabilitation. Arthroscopy. 2003;19:641-61.
10) Carlson HL, Haig AJ, Stewart DC. Snapping scapula syndrome: three case
reports and an analysis of the literature. Arch Phys Med Rehabil.
1997;78:506-11.
11) Warner JJ, Micheli LJ, Arslanian LE, Kennedy J, Kennedy R.
Scapulothoracic motion in normal shoulders and shoulders with glenohumeral
instability and impingement syndrome. A study using Moir´e topographic
analysis. Clin Orthop Relat Res. 1992;285:191-9.
12) Millett PJ, Pacheco IH, Gobezie R, Warner JJP. Management of
recalcitrant scapulothoracic bursitis: endoscopic scapulothoracic bursectomy
and scapuloplasty. Tech Shoulder Elbow Surg. 2006;7:200-5.
13) Groh GI, Simoni M, AIIen T, Dwyer T, Heckman MM, Rockwood CA Jr.
Treatment of snapping scapula with a periscapular muscle strengthening
program [abstract]. J Shoulder Elbow Surg. 1996;5(2-Pt 2):S6.
14) Kibler WB, Livingston B. Closed-chain rehabilitation for upper and lower
extremities. J Am Acad Orthop Surg. 2001;9:412-21.
15) Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder
pain. J Am Acad Orthop Surg. 2003;11:142-51
16) McQuade K, Dawson J, Schmidt G. Scapulothoracic muscle fatigue
associated with alterations in scapulohumeral rhythm. J Orthop Sports Phys
Ther. 1998;28:74-80.
17) Manske RC, Reiman MP, Stovak ML. Nonoperative and operative management
of snapping scapula. Am J Sports Med. 2004;32(6)1554-1565.
18) Saboeiro GR, Sofka CM. Imaging-guided treatment of scapulothoracic
bursitis. HSS J. 2007;3:213-5.
19) Nicholson GP, Duckworth MA. Scapulothoracic bursectomy for snapping
scapula syndrome. J Shoulder Elbow Surg. 2002;11:80-5.
20) McCluskey GM III, Bigliani LU. Surgical management of refractory
scapulothoracic bursitis. Orthop Trans. 1991;15:801.


 Snapping
scapula syndrome, or otherwise known as scapulothoracic crepitus, is
a disorder in which scapulothoracic motion produces a snapping,
grinding, thumping or popping sensation (1, 2). The sound is produced
by a tactile-acoustic phenomenon of which there exist a multitude of
potential causes ranging from bone spurs to muscular weakness to
bursitis (2). While most patients experience “snapping scapula” as
merely an annoying, asymptomatic crepitus, some do report a direct
correlation between the sound and the onset of pain, which can
result in a truly disabling condition (1).
Snapping
scapula syndrome, or otherwise known as scapulothoracic crepitus, is
a disorder in which scapulothoracic motion produces a snapping,
grinding, thumping or popping sensation (1, 2). The sound is produced
by a tactile-acoustic phenomenon of which there exist a multitude of
potential causes ranging from bone spurs to muscular weakness to
bursitis (2). While most patients experience “snapping scapula” as
merely an annoying, asymptomatic crepitus, some do report a direct
correlation between the sound and the onset of pain, which can
result in a truly disabling condition (1).  It is important to note that the scapulothoracic joint is not a true
synovial joint, yet merely an articulation between the anterior
scapula and the posterior thoracic cage with no attachment by
fibrous, synovial or cartilaginous tissue (3). This pseudo-joint
between the scapula and the thoracic cage is the most incongruent
articulation in the body, yet plays a crucial role in upper
extremity function and provides a stable base for glenohumeral
motion. This simultaneous, coordinated movement between the
scapulothoracic and glenohumeral joint produces what is known as
“scapulohumeral rhythm”, which consists of a motion ratio of 2° of
glenohumeral elevation to every 1° of scapulothoracic elevation.
Movement occurs along the plane of the scapula, which axes lie
30°-40° in frontal plane and 10°-20° anterior from vertical plane
(4).
Scapular function is mostly maintained through dynamic muscular
control of the following surrounding musculature: pectoralis minor,
coracobrachialis, serratus anterior, triceps, biceps, subscapularis,
rhomboids, levator scapulae, trapezius, deltoid, supraspinatus,
infraspinatus, teres minor, teres major, latissimus dorsi and
omohyoid (5).
It is important to note that the scapulothoracic joint is not a true
synovial joint, yet merely an articulation between the anterior
scapula and the posterior thoracic cage with no attachment by
fibrous, synovial or cartilaginous tissue (3). This pseudo-joint
between the scapula and the thoracic cage is the most incongruent
articulation in the body, yet plays a crucial role in upper
extremity function and provides a stable base for glenohumeral
motion. This simultaneous, coordinated movement between the
scapulothoracic and glenohumeral joint produces what is known as
“scapulohumeral rhythm”, which consists of a motion ratio of 2° of
glenohumeral elevation to every 1° of scapulothoracic elevation.
Movement occurs along the plane of the scapula, which axes lie
30°-40° in frontal plane and 10°-20° anterior from vertical plane
(4).
Scapular function is mostly maintained through dynamic muscular
control of the following surrounding musculature: pectoralis minor,
coracobrachialis, serratus anterior, triceps, biceps, subscapularis,
rhomboids, levator scapulae, trapezius, deltoid, supraspinatus,
infraspinatus, teres minor, teres major, latissimus dorsi and
omohyoid (5).