|
Conditions & Treatments - Adhesive Capsulitis - Frozen Shoulder |
|||||||||||||||||||||||||
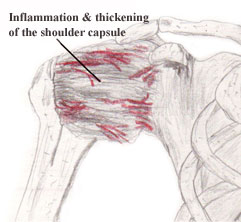
Adhesive capsulitis, commonly
termed "frozen shoulder," is a complicated, painful condition in which a patient
presents with shoulder pain and develops a gradual loss of both active and
passive shoulder range of motion (1). Adhesive capsulitis occurs in
approximately 2-5% of the population and is more prevalent in females,
individuals age 40-65, and those who have had a prior episode of adhesive
capsulitis in the opposite shoulder (1). Two types of adhesive capsulitis exist:
primary idiopathic adhesive capsulitis and secondary adhesive capsulitis.
Secondary adhesive capsulitis may be related to systemic disease (diabetes
mellitus and thyroid disorders) or a variety of intrinsic or extrinsic factors
(stroke, proximal humeral fracture, causative rotator cuff, and labral
pathology) (2).
|
Clinical Examination
Patients may report having difficulty maintaining a lying position, putting on clothes, taking off clothes, and reaching (2). Patients may also report having trouble completing daily routines, lifting, carrying, throwing, climbing, swimming, bathing, caring for their hair, cleaning, or completing a variety of other activities (2). Patients may exhibit a flexed posture and rounded shoulders (3). During ambulation, arm swing may be limited or absent (3).
Clinicians should ask patients questions regarding their ability to sleep through the night (ability to sleep indicates lower irritability) and if the chief complaint is pain or stiffness (to help determine staging) (3). Clinicians should also have patients fill out a validated functional outcome measure, such as the DASH, the ASES, or the SPADI (2). Clinicians should measure AROM and PROM, assess pain, and assess glenohumeral joint accessory motion (2).
Treatment Recommendations
In May 2013, Clinical Practice Guidelines were published for the treatment of adhesive capsulitis. The following table is a summary of the intervention guidelines presented in the article (2).
Table 2: Recommendations for the treatment of adhesive capsulitis from the Clinical Practice Guidelines.
| Intervention | Description | Recommendation Based On |
| Corticosteroid injections | When combined with shoulder mobility and stretching exercises, more effective in short term pain reduction than shoulder mobility and stretching exercises alone | Strong evidence |
| Patient Education | Clinicians should describe the course of the disease, promote activity modification, and match the intensity of intervention to the patient's current irritability level | Moderate evidence |
| Modalities | Short wave diathermy, ultrasound, electrical stimulation in addition to mobility and stretching exercises to reduce pain and increase ROM | Weak evidence |
| Joint Mobilization | Mobilizations primarily at the glenohumeral joint to reduce pain and increase ROM | Weak evidence |
| Translational Manipulation | Translational manipulation under anesthesia at the glenohumeral joint in patients not responding to conservative treatment | Weak evidence |
| Stretching Exercises | Stretching exercises at an intensity appropriate for the irritability level of the patient | Moderate evidence |
Research since the creation of the Clinical Practice Guidelines has continued to support the inclusion of static stretching in the treatment of adhesive capsulitis. In a study by Ibrahim et al. (4), sixty patients with adhesive capsulitis were randomly assigned to a treatment group or a control group. Both groups received 3 PT sessions/wk for 4 weeks; however, the treatment group also used a static progressive stretch device (one 30 minute session per day for the first week, two 30 minute sessions per day for the second and third weeks, and three sessions per day for the fourth week). At baseline, no differences existed between the two groups. However, after the intervention, differences between the two groups were statistically significant. The treatment group had lower pain ratings, lower DASH scores, increased PROM shoulder abduction, increased PROM shoulder ER, and increased AROM shoulder abduction. The differences between the two groups persisted at a 12 month follow up (4).
Outcomes
Although mild to moderate mobility deficits and pain may persist 12-18 months after the onset of adhesive capsulitis, many patients report minimal to no disability (2). 27-50% of patients report having mild symptoms 2-7 years after the onset of adhesive capsulitis (3). It is important to note that patients with diabetes mellitus may experience worse outcomes (2).
Last revised: July 20, 2014
by Michelle Kornder, DPT
References
1) Lynch TS and Edwards SL. Adhesive
capsulitis: current concepts in diagnosis and treatment. Current Orthopaedic
Practice. 2013;24(4):365-369. Available from University of Wisconsin
Madison, Madison, WI. Accessed July 7, 2014.
2) Kelley MJ, Shaffer MA, Kuhn JE et al. Shoulder Pain and Mobility
Deficits: Adhesive Capsulitis. J Orthop Sports Phys Ther. 2013;43(5):A1-A31.
Available from University of Wisconsin Madison, Madison, WI. Accessed July
7, 2014.
3) Hallisy, Thein-Nissenbaum. PT 677 -MS Dysfunction: Examination,
Diagnosis, & Management II. Madison, WI: Department of Physical Therapy;
2013.
4) Ibrahim M, Donatelli R, Hellman M, Echternach J. Efficacy of a static
progressive stretch device as an adjunct to physical therapy in treating
adhesive capsulitis of the shoulder: a prospective, randomised study
[published online ahead of print 2013]. Physiotherapy. Available from
University of Wisconsin Madison, Madison, WI. Accessed July 7, 2014.
5) Frozen Shoulder-OrthoInfo-AAOS. American Academy of Orthopaedic Surgeons.
Updated January, 2011. http://orthoinfo.aaos.org/topic.cfm?topic=a00071.
Accessed July 7, 2014.
6) Standard of Care: Shoulder Adhesive Capsulitis. Brigham and Women's
Hospital. Updated 2010. http://www.brighamandwomens.org/patients_visitors/pcs/rehabilitationservices/physical%20therapy%20standards%20of%20care%20and%20protocols/shoulder%20-%20adhesive%20capsulitis.pdf.
Accessed July 7, 2014.
7) Physical Therapist's Guide to Frozen Shoulder (Adhesive Capsulitis).
American Physical Therapy Association Move Forward Guide. http://www.moveforwardpt.com/SymptomsConditionsDetail.aspx?cid=00661806-1fa0-4fc0-ba17-ea32751d7412#.U7sFD_ldVBY.
Accessed July 7, 2014.
|
|
|
|






