The purpose of this case study was to illustrate the effects of combining
pulsetile lavage and vacuum assisted closure dressing for the treatment of a
surgical wound infection. Case Description: The patient was an 81 year
old male who underwent abdominal surgery which became infected. The patient was
sent to physical therapy for wound care for pulse lavage and sharp debridement
prior to application of vacuum assisted closure, three times a week. Outcome:
Measurements were taken during the initial evaluation and once a week during the
treatment period. The wound displayed dramatic results in percent of total wound
area closure and decreased necrotic tissue as a result of the combination of all
three forms of debridement. Discussion: The physical therapy plan of care
assisted wound closure in a shorter period of time when compared to normative
wound healing timeframes. A combination of different forms of debridement
provided a clean, moist, and sterile environment to enhance new granulated
tissue formation, allowing full wound closure.
The art of wound care is a trial and error science. There
are over 3000 different wound care products on the market that may be utilized
to treat patients. One of the forms of assisting wound closure is the vacuum
assistive closure device (VAC). The VAC consisted of a piece of foam placed
directly over and in the wound. Transparent tape is placed over the area
surrounding the wound to secure the foam and aids with draining the wound to
keep the area clean and sterile. Attached to the foam is a tube which removes
the drainage from the wound bed. The tube is connected to a vacuum source which
pulls the drainage from the wound into a disposable canister. The purpose of the
machine is to drain the excess fluid from the wound that may hinder the healing
process.
Another common treatment option for wound care is pulsetile lavage. This form of
mechanical debridement uses intermittent and pulsed jets of saline solution into
the wound bed and simultaneously suctions the debris from the wound. The process
helps loosen the debris from within the wound bed, reduce bacteria, and has the
ability to irrigate tunneling and undermining, common with many wounds.
Pulsetile lavage is a more specific form of debridement when compared to
whirlpool due to its ability to concentrate on a small area with the suction
tube.
The common factor with all wound care is a mixture of different forms of
debridement, ointments, and dressings. Finding this effective combination can
prove to be difficult, but by trial and error, a treatment plan can be created
with successful outcomes. This case report describes the combination of
different forms of wound care options as treatment for a surgically infected
abdominal wound. The following data describes the effectiveness of combining
pulsetile lavage, VAC, and sharp debridement as the primary treatment plan.
Case Description
Patient
The patient selected for the study presented to the hospital’s in-patient wound
care clinic with a large infected abdominal wound from a surgical procedure two
weeks prior. The patient was an 81 year old male who was retired and lived alone
at home. He was admitted to the hospital for transitional cell carcinoma. The
patient underwent a radical nephrourecterectomy, cystectomy, prostatectomy, and
urinary diversion surgery by way of abdominal entrance. Post surgery, the wound
became infected with bacteria and opened with necrotic tissue present. The
patient’s past medical history consisted of congestive heart failure, myocardial
infarct, cardiac artery disease, cardiac artery bypass graft surgery, renal
failure, change in mental status, cancer of the bladder, hypertension, diabetes
mellitus, hypercholestrecolemit, peripheral vascular disease, and sepsis. The
patient was at risk for falling due to pervious falls and his need for an
assistive device. The patient presented to the department as alert and had good
awareness to safety. He was independent at home with all functional activities
of daily living (ADLs) prior to hospital admission. He required the use of a
cane when ambulating short distances in and around his home and used a
wheelchair for long distances.
Three weeks after the surgery, an order was written by the
patient’s surgeon to send the patient to the physical
therapy department on Monday, Wednesday, and Friday for
pulse lavage to abdominal wound before the Vacuum Assistive
Device (VAC) dressing change. Prior to participating in the
study, the patient signed an informed consent form approved
by the hospital. The form allowed the author to take
photographs of the wound and access to all chart
information. No identifying information was allowed outside
the hospital.
Evaluation
 The initial evaluation took place in the physical therapy
wound care clinic. The evaluation consisted of a chart
review, wound inspection, measurements, wound description,
determining short and long term goals, developing the plan
of care, and patient education. The site of the wound was
midline of the body in the middle abdominal area. The wound
was considered full by the depth. Wound size measured to be
a width of 2.7cm, length 11.5cm, and depth 2.7cm. While
inspecting the edges within the wound, tunneling was found
at 12:00, most proximal, going 5.2cm superior. Necrotic
tissue within the wound bed was approximately 25% of the
entire wound surface. There was erythema noted around the
wound surface. No odor was present. Drainage was minimal,
consisting of blood. The infection was bactermia. Short and
long term goals were then decided. Short term goals were to
be accomplished by 2-4 weeks. These consisted of decreasing
the size of the wound by 25%, decreasing the amount of
necrotic tissue by 50%, and preparing the patient for
possible surgical intervention for closure of the wound.
Long term goals were to be met within 6-8 weeks. These
consisted of decreasing the size of the wound by greater
than 50% and decreasing amount of necrotic tissue by 100%.
Plan of care was determined, with physical therapy three
times a week; Monday, Wednesday, and Friday and to provide
patient and family education. Interventions included
pulsetile lavage with 2000ml of saline solution, sharp
debridement with scissors and forceps as needed, and
redressing of VAC dressing by the endointestinal nurse. The initial evaluation took place in the physical therapy
wound care clinic. The evaluation consisted of a chart
review, wound inspection, measurements, wound description,
determining short and long term goals, developing the plan
of care, and patient education. The site of the wound was
midline of the body in the middle abdominal area. The wound
was considered full by the depth. Wound size measured to be
a width of 2.7cm, length 11.5cm, and depth 2.7cm. While
inspecting the edges within the wound, tunneling was found
at 12:00, most proximal, going 5.2cm superior. Necrotic
tissue within the wound bed was approximately 25% of the
entire wound surface. There was erythema noted around the
wound surface. No odor was present. Drainage was minimal,
consisting of blood. The infection was bactermia. Short and
long term goals were then decided. Short term goals were to
be accomplished by 2-4 weeks. These consisted of decreasing
the size of the wound by 25%, decreasing the amount of
necrotic tissue by 50%, and preparing the patient for
possible surgical intervention for closure of the wound.
Long term goals were to be met within 6-8 weeks. These
consisted of decreasing the size of the wound by greater
than 50% and decreasing amount of necrotic tissue by 100%.
Plan of care was determined, with physical therapy three
times a week; Monday, Wednesday, and Friday and to provide
patient and family education. Interventions included
pulsetile lavage with 2000ml of saline solution, sharp
debridement with scissors and forceps as needed, and
redressing of VAC dressing by the endointestinal nurse.
Intervention
The typical treatment session consisted of the patient
arriving to the wound care department on a stretcher by the
hospital’s transportation department. A review of the
patient’s chart was conducted to insure no new changes in
the patient’s status which would contraindicate physical
therapy. The patient was taken back into the treatment area.
First, the VAC machine was turned to off and the dressing
would be removed. Once all dressings were removed,
inspection of the wound took place to note any
changes/improvements. The therapist performed pulse lavage
to all areas of the wound bed and tunneling with 2000ml of
saline solution. Sharp debridement of the necrotic tissue
from the base of the wound bed was performed, as needed,
with scissors and forceps. The wound was then redressed with
the VAC dressings by the endointestinal nurse. The patient
returned to his room on the stretcher via hospital
transportation.
Outcomes
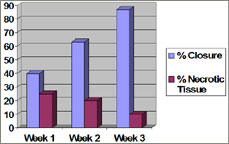 Measurements
of the wound were taken once a week and the change in total
percent of wound closure and total percent of decreased
necrotic tissue is illustrated on the graph. After week one
of treatment, the wound measured 10.0 cm in length, 2 cm in
width, 2.5 cm in depth, and the tunneling proximal at 12:00
to be 4.3 cm. The amount of necrotic tissue did not show a
significant decrease. Measurements
of the wound were taken once a week and the change in total
percent of wound closure and total percent of decreased
necrotic tissue is illustrated on the graph. After week one
of treatment, the wound measured 10.0 cm in length, 2 cm in
width, 2.5 cm in depth, and the tunneling proximal at 12:00
to be 4.3 cm. The amount of necrotic tissue did not show a
significant decrease.
The patient was reevaluated two weeks later. The chart
review contained the same information. New measurements were
taken of the wound, width was 1.5 cm, length 9.0 cm, depth
2.3 cm, and the 12:00 tunneling 3.4 cm going proximal.
Erythema was still present in the periwound and there was
minimum drainage of blood. After two weeks of treatment, the
wound had closed 1.2 cm in the width, 2.5 cm of the length,
0.4 cm in depth, and 2.8 cm in the tunneling. The overall
closure of the wound equaled 37%, which had met our short
term goal of 25% decrease in size of wound. The goal for
necrotic tissue was not met at this time.
 After the third week, the wound was again remeasured. A
bridge of new granulation tissue had formed in the center of
the wound 3.0 cm long, splitting the wound into two separate
areas. The proximal wound measured 3.5 cm in length, 1.2 cm
in width, and 2.0 cm in depth. The distal wound measured 1.5
cm in length, 1.0 cm in width, and 1.5 cm in depth. Necrotic
tissue had decreased to approximally 10% of total wound
area. After the third week, the wound was again remeasured. A
bridge of new granulation tissue had formed in the center of
the wound 3.0 cm long, splitting the wound into two separate
areas. The proximal wound measured 3.5 cm in length, 1.2 cm
in width, and 2.0 cm in depth. The distal wound measured 1.5
cm in length, 1.0 cm in width, and 1.5 cm in depth. Necrotic
tissue had decreased to approximally 10% of total wound
area.
The following week the patient was discharged from physical
therapy wound care secondary to partial closure of wound and
no further need for physical therapy care. The VAC will be
changed 3 times a week on the floor by the floor nurse for
the remainder of his hospital stay until the wound is fully
closed.
Discussion
Following the 4 week period of skilled wound care by
physical therapy of 3 times a week, the patient’s wound size
and necrotic tissue decreased significantly. This case
report displayed the course of treatment which produced
these results. The outcome suggested a combination of
different forms of debridement as treatment options can
produce a significant amount of closure in a wound which
could take up to 8 months for fully close and heal. The
amount of wound closure and decreased necrotic tissue was a
remarkable result for this type of wound and patient.
For the majority of wounds to close, the wound must stay
clean, moist, and free of excess exudate which can hinder
and lengthen the amount of time to heal. The average time
for a wound of this nature to close is up to 8 months. The
amount of time it took for this wound to heal is
significantly faster when compared to the normal timeframe.
The increase in healing time can be associated with the
combination of cleaning the wound with pulse lavage,
debriding the necrotic tissue to allow new tissue to
granulate, and keeping the area free of exudate by the VAC.
From this report, further research is needed to show the
effectiveness of these treatments together. Today, there is
little evidence on the effectiveness of the VAC dressing. I
believe this method when combined with other forms of
debridement and dressings are essential for wound care.
Last revised: June 8, 2009
by Sarah Wozny, DPT, CSCS
|


 The initial evaluation took place in the physical therapy
wound care clinic. The evaluation consisted of a chart
review, wound inspection, measurements, wound description,
determining short and long term goals, developing the plan
of care, and patient education. The site of the wound was
midline of the body in the middle abdominal area. The wound
was considered full by the depth. Wound size measured to be
a width of 2.7cm, length 11.5cm, and depth 2.7cm. While
inspecting the edges within the wound, tunneling was found
at 12:00, most proximal, going 5.2cm superior. Necrotic
tissue within the wound bed was approximately 25% of the
entire wound surface. There was erythema noted around the
wound surface. No odor was present. Drainage was minimal,
consisting of blood. The infection was bactermia. Short and
long term goals were then decided. Short term goals were to
be accomplished by 2-4 weeks. These consisted of decreasing
the size of the wound by 25%, decreasing the amount of
necrotic tissue by 50%, and preparing the patient for
possible surgical intervention for closure of the wound.
Long term goals were to be met within 6-8 weeks. These
consisted of decreasing the size of the wound by greater
than 50% and decreasing amount of necrotic tissue by 100%.
Plan of care was determined, with physical therapy three
times a week; Monday, Wednesday, and Friday and to provide
patient and family education. Interventions included
pulsetile lavage with 2000ml of saline solution, sharp
debridement with scissors and forceps as needed, and
redressing of VAC dressing by the endointestinal nurse.
The initial evaluation took place in the physical therapy
wound care clinic. The evaluation consisted of a chart
review, wound inspection, measurements, wound description,
determining short and long term goals, developing the plan
of care, and patient education. The site of the wound was
midline of the body in the middle abdominal area. The wound
was considered full by the depth. Wound size measured to be
a width of 2.7cm, length 11.5cm, and depth 2.7cm. While
inspecting the edges within the wound, tunneling was found
at 12:00, most proximal, going 5.2cm superior. Necrotic
tissue within the wound bed was approximately 25% of the
entire wound surface. There was erythema noted around the
wound surface. No odor was present. Drainage was minimal,
consisting of blood. The infection was bactermia. Short and
long term goals were then decided. Short term goals were to
be accomplished by 2-4 weeks. These consisted of decreasing
the size of the wound by 25%, decreasing the amount of
necrotic tissue by 50%, and preparing the patient for
possible surgical intervention for closure of the wound.
Long term goals were to be met within 6-8 weeks. These
consisted of decreasing the size of the wound by greater
than 50% and decreasing amount of necrotic tissue by 100%.
Plan of care was determined, with physical therapy three
times a week; Monday, Wednesday, and Friday and to provide
patient and family education. Interventions included
pulsetile lavage with 2000ml of saline solution, sharp
debridement with scissors and forceps as needed, and
redressing of VAC dressing by the endointestinal nurse.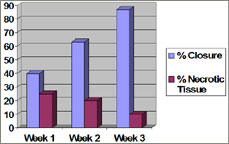 Measurements
of the wound were taken once a week and the change in total
percent of wound closure and total percent of decreased
necrotic tissue is illustrated on the graph. After week one
of treatment, the wound measured 10.0 cm in length, 2 cm in
width, 2.5 cm in depth, and the tunneling proximal at 12:00
to be 4.3 cm. The amount of necrotic tissue did not show a
significant decrease.
Measurements
of the wound were taken once a week and the change in total
percent of wound closure and total percent of decreased
necrotic tissue is illustrated on the graph. After week one
of treatment, the wound measured 10.0 cm in length, 2 cm in
width, 2.5 cm in depth, and the tunneling proximal at 12:00
to be 4.3 cm. The amount of necrotic tissue did not show a
significant decrease. After the third week, the wound was again remeasured. A
bridge of new granulation tissue had formed in the center of
the wound 3.0 cm long, splitting the wound into two separate
areas. The proximal wound measured 3.5 cm in length, 1.2 cm
in width, and 2.0 cm in depth. The distal wound measured 1.5
cm in length, 1.0 cm in width, and 1.5 cm in depth. Necrotic
tissue had decreased to approximally 10% of total wound
area.
After the third week, the wound was again remeasured. A
bridge of new granulation tissue had formed in the center of
the wound 3.0 cm long, splitting the wound into two separate
areas. The proximal wound measured 3.5 cm in length, 1.2 cm
in width, and 2.0 cm in depth. The distal wound measured 1.5
cm in length, 1.0 cm in width, and 1.5 cm in depth. Necrotic
tissue had decreased to approximally 10% of total wound
area.




