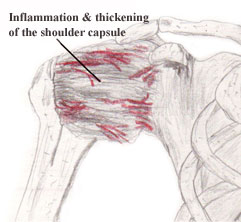
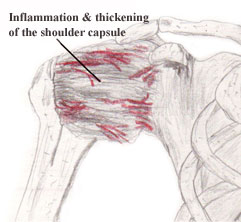
Adhesive capsultis is also
known as periarthritis or frozen shoulder syndrome and is characterized by
diffuse shoulder pain and loss of motion. It usually involves regional
tightness in the anteroinferior joint capsule which primarily compromises
external rotation, followed by loss of abduction and, less often internal
rotation and flexion (1). The exact pathogenesis of adhesive capsulitis is
unclear (2,3,4) but Yang et al (3) revealed that several authors have
proposed that impaired shoulder movements are related to shoulder capsule
adhesions, contracted soft tissues, and adherent axillary recess.
Patients with adhesive capsulitis are treated conservatively with
nonsteroidal anti-inflammatory drugs, intra-articular cortisocosteriod
injections and physical therapy (4). Should conservative treatment methods
prove ineffective more aggressive methods such as hydrodilation,
arthroscopic release, or manipulation under anesthesia can be performed (4).
In the physical therapy setting, physical therapists utilize a variety of
interventions to treat patients with adhesive capsulitis. These
interventions can include and are not limited to: active/passive range of
motion exercises, stretching, soft tissue mobilization, myofascial release,
proprioceptive-neuromuscluar techniques, ultrasound, electrical stimulation,
hot packs, ice packs and joint mobilization techniques.
 In this article we will focus on joint mobilization for the treatment of
adhesive capsulitis of the shoulder. A leading researcher in joint mobilization technique is
Geoffrey Maitland. He reported that joint mobilization is most effective
when directed to restoring structures within a joint to their normal
positions or pain-free positions so as to allow a full-range painless
movement; stretching a stiff painless joint to restore range, and relieving
pain by using special techniques (5). Maitland classifies joint mobilization
techniques into five grades: In this article we will focus on joint mobilization for the treatment of
adhesive capsulitis of the shoulder. A leading researcher in joint mobilization technique is
Geoffrey Maitland. He reported that joint mobilization is most effective
when directed to restoring structures within a joint to their normal
positions or pain-free positions so as to allow a full-range painless
movement; stretching a stiff painless joint to restore range, and relieving
pain by using special techniques (5). Maitland classifies joint mobilization
techniques into five grades:
| Intensity of
Mobilization Techniques According to Maitland 5-Grade Classification
System (5) |
| Grade I: |
Small amplitude at the beginning of
the range of motion (ROM) |
| Grade II: |
Large amplitude not reaching the end
of the ROM |
| Grade III: |
Large amplitude reaching the limited
ROM |
| Grade IV: |
Small amplitude at the end of the
limited ROM |
| Grade V: |
Small amplitude and high velocity at
the end of limited ROM (manipulation or thrust) |
Joint mobilization is an often used intervention by physical therapists to
treat patients with adhesive capsultis. Yang et al (3) conducted a study
that compared the use of three mobilization techniques – end-range
mobilization, mid-range mobilization, and mobilization with movement in the
management of 28 subjects with adhesive capsulitis. Their study concluded
that there was improvement in mobility and functional ability at 12 weeks in
subjects treated with the three mobilization techniques. When comparing the
effectiveness of the three treatment strategies in subjects with unilateral
adhesive capsultis, they found that end-range mobilization and mobilization
with movement were more effective than mid-range mobilization in increasing
mobility and functional ability.
In a preliminary study by Vermeulen et al (6) published in 2000, they
conducted a study on four men and three women with adhesive capsulitis who
were treated with end-range mobilization techniques, twice a week for 3
months. Their study found that after 3 months of treatment, there were
increases in both active range of motion and passive range of motion.
However, their study didn’t include a control group and they recommended
that further investigation in the form of controlled studies is warranted to
compare the therapeutic effect of these mobilizations with the natural
course of the disease or other treatment regimes.
In a later study by Vermeulen et al (4) published in 2006, they conducted a
study on 100 subjects with unilateral adhesive capsulitis who were randomly
divided into two groups and were treated with either high-grade mobilization
techniques or low-grade mobilization techniques. Their study found that
high-grade mobilization techniques proved to be more effective than
low-grade mobilization techniques with improving glenohumeral joint mobility
and reducing disability, with the overall differences between the two
interventions being small.
Despite the positive findings with the above mentioned studies, the
inclusion of a control group where no treatment is received by patients with
adhesive capsulitis was not included in any of the studies. Because the
natural course of this condition remains a matter of dispute future studies
involving a control group and a larger sample population are recommended
(4).
|
A review of some shoulder mobilization techniques to the Glenohumeral
(GH) joint
can be found below (7)
(please note that there are alternative methods to
performing these mobilizations): |

Anterior Glide
of the GH Joint - While supporting the patient's forearm between
your upper arm and trunk, apply a grade I traction at the GH joint
with the guiding hand while the mobilizing hand glides the humerus
in an anterior direction.
|
| |

Posterior Glide
of the GH Joint - While supporting the patient's forearm between
your upper arm and trunk, apply a grade I traction to the GH joint
with the guiding hand while the mobilizing hand glides the humerus
in a posterior direction.
|
| |

Inferior Glide
of the GH Joint - While supporting the patient's forearm between
your upper arm and trunk, apply a grade I traction to the GH joint
with the guiding hand while the mobilizing hand glides the humerus
in an inferior direction.
|
| |

Distraction of
the GH Joint - While
supporting the patient's forearm between your upper arm and trunk,
grip the proximal humerus as close to the axilla as possible from
the medial and lateral side with both hands and move the humeral
head lateral, anterior and inferior, perpendicular to the glenoid
joint surface.
|
Last revised: November 15, 2009
by Jennifer Hill, MPT, CSCS & Chai Rasavong, MPT, MBA
References
1.
Goodman, C & Boissonnault W. Pathology: Implications for the Physical
Therapist. Philadelphia, PA: WB Saunders, 1998.
2.
Wadsworth, C. Frozen Shoulder. Physical Therapy. 1986;66(12): 1878-1883.
3.
Yang J., et al. Mobilization Techniques in Subjects with Frozen Shoulder
Syndrome: Randomized Multiple-Treatment Trial. Physical Therapy.
2007;87(10): 1307-1315.
4.
Vermeulen H., et al. Comparison of High-Grade and low-Grade Mobilization
Techniques in the Management of Adhesive Capsultis of the Shoulder:
Randomized Controlled Trial. Physical Therapy. 2006;86(3): 355-368.
5
Maitland GD. Peripheral Manipulation. Boston, MA: Butterworth Publishers;
1977.
6.
Vermeulen H, et al. End-Range Mobilization Techniques in Adhesive Capsultis
of the Shoulder Joint: A Multiple-Subject Case Report. Physical Therapy.
2000;80(12): 1204-1213.
7. Edmond, S. Joint Mobilization/Manipulation - Extremity and Spinal
Techniques Second Edition. St. Louis, MO: Mosby Elsevier, 2006. |


 In this article we will focus on joint mobilization for the treatment of
adhesive capsulitis of the shoulder. A leading researcher in joint mobilization technique is
Geoffrey Maitland. He reported that joint mobilization is most effective
when directed to restoring structures within a joint to their normal
positions or pain-free positions so as to allow a full-range painless
movement; stretching a stiff painless joint to restore range, and relieving
pain by using special techniques (5). Maitland classifies joint mobilization
techniques into five grades:
In this article we will focus on joint mobilization for the treatment of
adhesive capsulitis of the shoulder. A leading researcher in joint mobilization technique is
Geoffrey Maitland. He reported that joint mobilization is most effective
when directed to restoring structures within a joint to their normal
positions or pain-free positions so as to allow a full-range painless
movement; stretching a stiff painless joint to restore range, and relieving
pain by using special techniques (5). Maitland classifies joint mobilization
techniques into five grades: