With a standard
total shoulder arthroplasty (TSA) it
relies on an intact rotator cuff to control the humeral
component much like the native shoulder. Because of superior
humeral head migration, eccentric loading on the glenoid
component resulted in a “rocking-horse” motion and loosening
of the glenoid component. As a result of this loosening,
this procedure would be abandoned for a more yielding
procedure, the reverse total shoulder arthroplasty.

The reverse total shoulder arthroplasty was first
developed in Europe by Paul Grammont and was approved in the
US by the FDA in March of 2004. With this procedure, the
socket and metal ball are switched in the joint. This
involves a metal ball being attached to the glenoid
component and a plastic socket being attached to the humeral
component. As a result of this design there is a small
lateral offset secondary to the absence of the component
neck which places the center of rotation more medially and
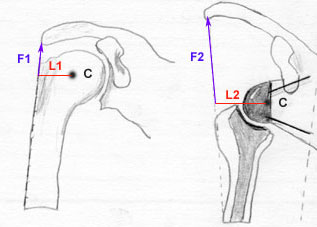
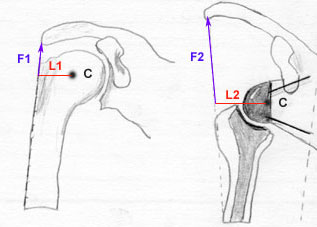
reduces the torque at the glenoid-bone interface. The lever
arm distance (L) is increased and deltoid force (F) is
increased by lowering and medializing the center of rotation
which is now also fixed. Torque (F x L) in abducting the arm is also
increased. (see image below)
|
 |
When examining the biomechanics involved with a reverse TSA
more closely, it is revealed that this procedure alters the
biomechanics of the shoulder by changing the position of the
humeral and glenoid components. The center of rotation of
the joint moves medially and inferiorly. Deltoid resting
muscle tone is increased to allow it to become the primary
mover for shoulder elevation in the presence of rotator cuff
dysfunction. This also allows the deltoid to provide
stability in a rotator cuff deficient
shoulder.
Indications for a reverse total shoulder arthoplasty
includes:
• Failed hemiarthroplasty with irreparable rotator cuff
tears
• Pseudoparalysis (i.e., inability to lift the arm above the
horizontal) because of massive, irreparable rotator cuff
tears
• Some reconstructions after tumor resection
• Some fractures of the shoulder (Neer three-part or
four-part fracture)
• Severe proximal humerus fractures with tuberosity
malposition or non-union
Contraindications for a reverse total shoulder
arthroplasty includes:
• Primary osteoarthritis or osteonecrosis where the
articular surface – tuberosity relationships are normal and
the rotator cuff is intact
• Marked deltoid deficiency, as the shoulder will not
function well and will be prone to dislocate
• History of previous infection – recurrent infection high
• Use sparingly in patients less than 65 years old, as
long-term survivorship and complication rates are unknown
Complication rates have been found to be higher
intraoperatively and postoperatively for reverse TSA (mean
24%) vs. conventional TSA (mean 15%). Besides cuff
arthropathy, reverse TSA are still regarded a salvage
procedure for failed hemiarthroplasties. If these salvage
procedures are excluded, the complication rate is less.
Recent postoperative or acute complications includes:
hematoma, dislocation, prosthesis loosening, infection,
periprosthetic fracture, and metaglene migration. Late
postoperative period or chronic complications includes:
scapular erosion, osteophyte formation, heterotopic
ossification and acromion or scapular stress fractures.
A potential complication for a reverse TSA is
anterior-superior dislocation as a result of unopposed pull
or inadequate tension of the deltoid muscle. It has also
been found that 20% of reverse TSA had dislocations in one
series. Shoulder dislocation precautions includes: no
shoulder motion behind back (NO combined shoulder
adduction, internal rotation, and extension), and no glenohumeral (GH) extension beyond neutral. (Precautions
should be implemented for 12 weeks postoperatively unless
surgeon specifically advises patient or therapist
differently)
The postoperative rehab protocol may vary from surgeon to
surgeon. Factors affecting rehabilitation can include: the
patient’s premorbid level of function, the type of
prosthetic utilized, bone stock, patient compliance post
operatively and the ability of patient to activate deltoid
postoperatively. Communication with the surgeon to discuss
post operative rehabilitation is imperative when working
with patients who have undergone this procedure. Internet
searches of rehab protocols have revealed a wide array of
slightly different takes from various surgeons for a post
operative protocol. The protocols appeared to differ mostly
on return to activity and progression from PROM to AAROM to
AROM. More research is needed to identify the most
efficacious post operative rehabilitation protocol following
Reverse TSA.
Below is a general protocol for reverse TSA which we
recommend to physical therapists who work with our patients:
Initial Stage
• From POD 1 to 6 weeks post operatively
• Maximum protection of joint
• Attain full PROM (educate family as to definition of PROM)
• Reinforce use of sling for 2-6 weeks post operatively
• AROM of elbow/wrist/hand
• Cryotherapy
Initial Stage Precautions
• In supine, arm should be supported by pillow to avoid
shoulder extension
• NO SHOULDER AROM
• No lifting or weight bearing
• Keep incision clean & dry
• No pools or jacuzzi for 4-6 weeks
Stage II (6-16 weeks)
• Increase PROM to tolerance
• Gently introduce AROM
• Continue modalities for inflammation reduction PRN
• Improve Scapular stability
• Avoid hyperextension
• Begin PROM internal rotation in plane of scapula
• 8-10 weeks initiate AAROM forward flexion, elevation, ER
and IR in plane of scapula in supine then progress to
sitting/standing
• 8-10 weeks initiate Sub-maximal isometrics for IR & ER
• 8-10 weeks initiate Deltoid and Scapular isotonic
exercises
• 10-14 weeks initiate AROM forward flexion and elevation in
plane of scapula with low resistance
• 10-14 weeks initiate AROM glenohumeral ER/IR (isotonics)
• By end of stage II, patient should possess ability to
recruit Deltoid as primary mover of shoulder
Stage III (16 weeks to one year)
• Continue to progress flexion and elevation with resistance
per patient tolerance
• Comprehensive HEP
• Gradual return to premorbid functional and recreational
activities within limits of precautions established by
surgeon and therapist
• D/C from PT when patient attains functional AROM (about
100 degrees elevation) with good shoulder arthrokinematics
• Progress isotonics as tolerated
• Continue to reinforce gradual return to activities such as
tucking in a shirt at 14 - 16 weeks to prevent dislocation
• Continue to improve upper quarter muscle strength
gradually over time to ensure successful post surgical
outcome
For more information about reverse total shoulder
arthroplasty please contact Dr. Clark of
South Shore
Orthopedic Surgery Group at
info@ss-ortho.com.
Last revised: October 16, 2011
by David Clark, MD