Proprioceptive
neuromuscular facilitation (PNF) is a physical therapy treatment
approach which utilizes functionally based movement patterns with
techniques of neuromuscular facilitation (1). The purpose of PNF is
to evoke motor responses and improve neuromuscular control and
function. Essentially, PNF is an advanced form of flexibility
training that involves both the stretching and contraction of the
muscle group being targeted (2). Numerous investigations establish
PNF techniques as more efficacious treatments than traditional
static stretching (3-6). It can be used throughout the entire
spectrum of rehabilitation, from employing isometrics in the
earliest phases of tissue healing to high-velocity, diagonal
patterns against maximum resistance in the later phases of
rehabilitation (1).
PNF techniques are used most frequently for injuries of the
shoulders, knees, hips, and ankles (4-8). These techniques are
utilized to assist with initiating range of motion, increasing range
of motion, decreasing pain, teaching a motion, strengthening,
promoting stability, facilitating proprioception, increasing
endurance and restoring function (9). The basic principles of PNF
include utilization of manual pressure, verbal cues, visual
stimulus, proprioceptive input, stretch, appropriate resistance,
patterns and timing in order to instruct a patient on a movement and
to achieve desired outcomes (9, 10). Manual pressure is
utilized to provide the appropriate tactile cue for the desired
direction of movement, while verbal cues are provided to
instruct the patient on the desired movement. Visual stimulus
allows the therapist to demonstrate to the patient how to perform a
movement and also allows the patient to have visual input and a
point of reference when performing the movement. Proprioceptive
input involves providing joint input to further enhance learning
of the movement. Traction or approximation of a joint are such
techniques that provide input to a joint. Providing a quick
stretch followed by resistance allows for firing of muscle
spindles to initiate/enhance motor responses and for facilitation to
occur (10). Providing the appropriate resistance (isotonic or
isometric) for a movement in a pain free range will allow for the
patient to move in a smooth coordinated fashion and can assist with
facilitating muscle response, muscle re-education and increasing
strength, endurance & coordination (10). Implementing various gross
functional patterns involving diagonal & rotational patterns
with PNF techniques can assist with achieving desired outcomes as
well. Lastly, timing allows for emphasis of the desired
sequence of muscle contraction to occur which results in coordinated
movement (10).
This article will review the PNF techniques that can be used in
rehabilitation of shoulder injuries, such as sprains, strains,
dislocations, instability, separations, tendinitis, bursitis, torn
rotator cuffs, frozen shoulder, and arthritis (4-10). A clinical
commentary written by Davies and Dickoff-Hoffman makes the point
that the shoulder joint is under a lot of demand (11). In order to
function properly, the shoulder joint requires both great
neuromuscular control and large amounts of motion. Davies and
Dickoff-Hoffman emphasize the importance of the following goals in
neuromuscular rehabilitation: 1 ) increase dynamic caudal glide
provided by the rotator cuff muscles, 2) increase range of motion of
the posterior capsule and flexibility of the posterior rotator cuff
muscles (infraspinatus and teres minor), and 3) strengthen the
posterior shoulder muscles (11).
Exercise, passive mobilization, and PNF are commonly used in the
treatment of shoulder joint pathologies (11-14). Studies have found
that range of motion increases and pain decreases after the
application of these treatment techniques (11-14). After a four week
period and twelve treatment sessions consisting of exercise, passive
mobilization, and PNF, patients (n=41) reported a mean improvement
of 30.0 degrees of flexion, 21.0 degrees of abduction, 12.0 degrees
of lateral rotation, and 10.5 degrees of medial rotation (12). Mean
decreases in pain of 2.9 points on the Numerical Pain Rating Scale (NPRS)
were also found (12). Another study, which was a randomized control
trial conducted by Godges et al. evaluated the immediate effect of
soft tissue mobilization (STM) with PNF to increase glenohumeral
external rotation (13). It was found that the treatment group gained
16.4 degrees of external rotation versus 1 degree gain in the
control group after just one session. The treatment consisted of
soft tissue mobilization of the subscapularis for 7 minutes, 5
repetitions of contract-relax to the shoulder internal rotators, and
5 repetitions of PNF facilitating flexion, abduction, and external
rotation diagonal (13).
Not only can PNF be used to rehabilitate shoulder injuries, but it
also can be used in performance training. A study conducted by
Decicco and Fisher (n=30) compared the effects of two different PNF
techniques, contract-relax-contract (CRC) and hold-relax-contract (HRC),
on shoulder ROM in overhand throwing athletes (14). These PNF
techniques were performed two times a week for six weeks. An
increase in shoulder external range of motion was found for both
intervention groups (CRC +14.6 degrees, HRC +13.5 degrees), but no
increase was found in the control group (14). No significant
difference in range of motion was noted between the two PNF
techniques.
When used alongside other treatment options such as exercise and
passive mobilization, PNF has been found to be efficacious in
shoulder rehabilitation (13-15). Indeed, further research is
warranted to include PNF only groups, which would allow for
conclusions to be made regarding the efficacy of PNF as a separate
treatment option for shoulder injuries.
Commonly used PNF techniques to rehabilitate shoulder conditions and
injuries include rhythmic initiation, hold relax, contract relax,
alternating isometrics, and slow reversals. See Below.
|
A review of common shoulder PNF techniques to rehabilitate shoulder
conditions (1, 15): |
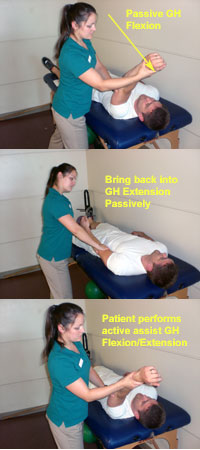
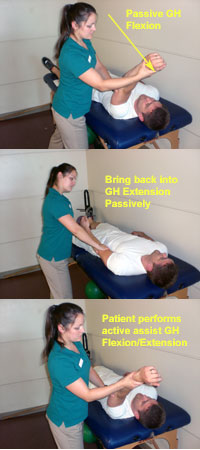
Rhythmic
Initiation - GH Fexion/Extension: PNF technique in which movement progresses from
completely passive to active assisted to slightly resisted as the
patient relaxes and is capable of actively moving. Works well with
the patient who is unable to initiate movement, or ROM is limited by
hypertonia, or has difficulty learning motor skills.
• Verbal command: “Relax and let me move your arm straight up and
back (GH flexion and extension).”
• As patient relaxes, “Now you do it with me.”
• Movement should be repetitive, slow and rhythmic. Avoid quick
stretch of any muscle group that should be relaxing.
• This technique can also be performed for other motions at the
shoulder including GH abduction, GH internal rotation, GH external
rotation, & PNF UE flexion D1 & D2 patterns.
|
| |

Hold Relax - GH
Flexion:
isometric PNF technique performed in the agonist pattern at the
point of limited range of motion. It is effective when ROM is
reduced because of muscle tightness on one side of the joint, or
when pain is part of the limitation.
• The limb is moved (active or passive) toward the point of
limitation (GH flexion).
• Isometric contraction for 7-9 seconds into the antagonist pattern
(GH extension).
• Patient relaxes (2-3 secs).
• Passive movement into the new range of the agonist pattern (GH
flexion) for a stretch of 10-15 seconds.
• Repeat until no further gain can be achieved.
• This technique can also be performed for other motions at the
shoulder including GH abduction, GH internal rotation, GH external
rotation, & PNF UE flexion D1 & D2 patterns.
|
| |

Contract Relax -
GH Flexion:
PNF technique performed in the agonist pattern used to gain range
when muscle tightness or guarding is limiting the motion required
for functional activities.
• The limb is moved (active or passive) toward the point of
limitation.
• Patient performs an isotonic contraction into available GH flexion.
• Isometric contraction for 7-9 seconds into the antagonist pattern
(GH extension).
• Patient relaxes (2-3 secs).
• Passive movement into the new range of the agonist pattern (GH
flexion) for a stretch of 10-15 seconds.
• Repeat until no further gain can be achieved.
• This technique can also be performed for other motions at the
shoulder including GH abduction, GH internal rotation, GH external
rotation, & PNF UE flexion D1 & D2 patterns.
|
| |

Alternating
Isometrics - GH Flexion/Extension: isometric contractions rhythmically on one side of
the GH joint then the other, with no relaxation occurring between
contractions. The goal is to increase endurance or strength to hold
a position. These are often done in midline or in weight bearing
positions. This technique can also be performed for other motions at
the shoulder including GH abduction, GH internal rotation, GH external
rotation, & PNF UE flexion D1 & D2 patterns.
|
|
|

Slow Reversals -
GH Flexion/Extension:
is slow, resisted rhythmical concentric contractions alternating
between the stronger GH agonist and the weaker GH antagonist muscle
groups without relaxation occurring between reversals. Quick stretch
can be applied in the lengthened range to initiate movement as
needed. This technique can also be performed for other motions at
the shoulder including GH abduction, GH internal rotation, GH external
rotation, & PNF UE flexion D1 & D2 patterns.
|
By implementing the principles and strategies of
PNF into rehabilitation of various shoulder injuries, physical therapists
will be able to promote the response of neuromuscular mechanisms and
ultimately return their patients to normal function. Whether promoting
flexibility, developing functional movement, developing muscular strength
and endurance, improving joint stability, or increasing neuromuscular
coordination and control, PNF can be incorporated into any physical therapy
setting as a valuable and efficacious component of rehabilitation.
Last revised: June 15, 2010
by Jennifer Werwie, SPT & Chai Rasavong, MPT, MBA
References
1. Kisner C, Colby LA. 2007. Therapeutic Exercise: Foundations and
Techniques. 5th edition. p. 195-203.
2. Walker B. PNF Stretching Explained- Proprioceptive Neuromuscular
Facilitation. The Stretching Institute. http://www.thestretchinghandbook.com/archives/pnf-stretching.php.
2010. Accessed: June 9, 2010.
3. Tanigawa MC. Comparison of the hold-relax procedure and passive
mobilization on increasing muscle length. Phys Ther. 1972; 52: 725-735.
4. Surburg, PR., Schrader, JW. Proprioceptive Neuromuscular Facilitation
Techniques in Sports Medicine: A Reassessment. Journal of Athletic Training.
1997; 32(1):34-39.
5. Gibson K, Growse A, Korda L, Wray E, MacDermis JC. The effectiveness of
rehabilitation for nonoperative management of shoulder instability: a
systematic review. Journal of hand therapy 2004 (2) 229-242.
6. Belling Sorensen AK, Jorgensen U. Secondary impingement in the shoulder,
an improved terminology in impingement. Scandinavian journal of medicine &
science in sports. 2000 (10) 266-278.
7. Casonato O, Musarra F, Frosi G, Testa M. The role of therapeutic exercise
in the conflicting and unstable shoulder. Physical Therapy Reviews 2003 (8)
69-84.
8. Callanan M, Tzannes A, Hayes K, Paxinos A, Walton J, Murrell GA. Shoulder
instability. Diagnosis and management. Australian family physician 2001 (7)
655-661.
9. Armitage D. Overview of Proprioceptive Neuromuscular Facilitation.
Athletic Orthopedics and Knee Center. http://www.aokc.net/SWAPPID/99/SubPageID/21814.
2007. Accessed: June 9, 2010.
10. Hagen N. 2010. Putting PNF into Practice. Madison, WI. University of
Wisconsin-Madison DPT Program. pp. 4-9.
11. Davies GJ, Dickoff-Hoffman S. Neuromuscular testing and rehabilitation
of the shoulder complex. J Orthop Sports Phys Ther. 1993; 18: 449-458.
12. Mahomed S, Al-Obaidi S, Al-Zoabi B. Outcome Measures and Psychomotor
Skills Related to Shoulder Conditions for Clinical Orthopedic Training. Med
Princ Pract. 2008; 7:481-485.
13. Godges JJ, Shah D, Thorpe D, Mattson-Bell M. The Immediate Effects of
Soft Tissue Mobilization With Proprioceptive Neuromuscular Facilitation on
Glenohumeral External Rotation and Overhead Reach. J Orthop Sports Phys Ther.
2003; 33(12):713-718.
14. Decicco PV, Fisher MM. The effects of proprioceptive neuromuscular
facilitation stretching on range of motion in overhand athletes. J Sports
Med Phys Fitness. 2005;45:183-187.
15. Dewane J. 2010. Foundations of Therapeutic Intervention: Integrating PNF
into Treatment Progression. Madison, WI. University of Wisconsin-Madison DPT
Program. pp. 7-9. |