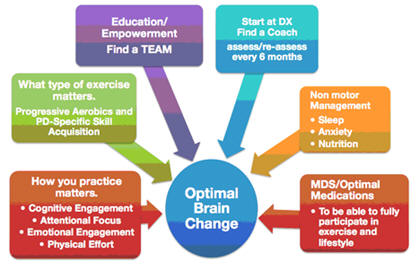
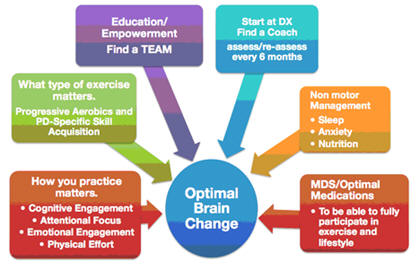
Research suggests that WHAT you do is important! The
WHAT you do should be about vigorous aerobic exercise
and Parkinson's Disease (PD) - specific skill training.
The skills that deteriorate in PD interfere with
everyday movement, therefore, movements become slow,
small, and poorly sequenced. To maintain or restore
those PD-specific skills, a PWR!4Life Program involves
the daily rehearsal of big and fast, whole body
functional movements – these are called the BASIC4 |
PWR!Moves. Studies suggest that the combination of these
types of exercise (aerobics and skill training) may
enhance learning and automaticity beyond what is
possible with either one alone!*
Finally, HOW you practice is essential to your ability
to GET BETTER and STAY BETTER. It is not enough to just
practice the same small and slow movements over and over
again without paying attention to the quality of the
movement. Instead, it is about improving the quality of
your practice, being engaged, and being challenged
physically and cognitively to DO MORE!
PWR!Moves is a PD-specific skill training program to
maintain or restore skills that deteriorate and
interfere with everyday movements.
Dr.
Farley created PWR!MovesŪ as the EVOLUTION of her
original LSVT BIGŪ exercise program. The BASIC4 |
PWR!MovesŪ offer a flexible and functional
amplitude-focused exercise approach that targets
multiple symptoms, and that allows for adaptation for
disease severity.
PWR!Moves can be combined and progressed into a
stand-alone group program or integrated into ANY
exercise program, ANY activity (function, activities of
daily living, recreation, sports, and hobbies), in ANY
setting (community group or rehab 1:1), by therapists
and fitness professionals.
The BASIC4 | PWR!Moves are performed with large
amplitude, high effort, and attention to action in
multiple postures (floor, all 4’s, sitting, and
standing). They specifically target “4” skills shown by
research to interfere with mobility in people with PD
(antigravity extension, weight shifting, axial mobility,
and transitional movements).
All of the BASIC4 | PWR!Moves may be performed
differently to specifically target different symptoms of
PD:
~ PREPARE ~To Counteract Rigidity: then PWR!Moves are
performed slowly, rhythmically and with sustained
effort.
~ Activate ~To Counteract Bradykinesia; then PWR!Moves
are performed as BIG and FAST as possible with
repetitive high effort.
~ Flow ~To Counteract Incoordination; then PWR!Moves are
linked together into gradually longer sequences that
mimic everyday movement and improve overall function in
LIFE.
~ Boosts ~To Counteract Loss of Automaticity; then
PWR!Moves are combined with secondary motor and
cognitive tasks to create real world environmental
context
PWR!4Life™ Program Essentials for Wellness Recovery
Exercise4BrainChange represents Dr. Farley’s translation
of the research about “how to exercise” to optimize
brain health (neuroprotection), brain change
(neuroplasticity) and function. There are “4” essential
constructs (high physical effort, cognitive engagement,
attentional focus, emotional engagement). The constructs
are founded on basic and clinical research in motor
control, motor learning, and exercise physiology.
About PWR!
The aim of PWR! is to use exercise as a physiological
tool to optimize brain function (i.e. neuroplasticity)
and health. Her program is based on: early intervention,
continuous access and research-based exercise programs.
PWR! also trains clinicians and fitness professional
with techniques to focus on PD-specific exercise.
Her exercise tips:
1 “start from a position of power!”. Your body needs to
be ready, your brain needs to be focused and the task
needs to feel important (or fun!) for change to occur.
Make your exercise engaging!
2 Use equipment (i.e. bungees, ropes, balance boards,
harnesses) to get the experience of the full movement
safely (especially in people with PD who have difficulty
balancing etc.), then start to take some of those
supports away as you progress and apply that experience
to everyday movements!
3 For people with PD, especially those with dyskinesias
– seek exercises that gain core stability
4 Sensory feedback – i.e. pacing, metronome, music – can
help push you to exercise faster, harder and with more
smooth movements
5 “Prime” your body by starting your exercise program
with progressive aerobic training, then follow up with
skill acquisition-type exercises.
6 Focus not only on increasing muscle mass, but want to
increase useable muscle and focus on functional
movements in your exercises… not just “curls for the
girls” but include things like:
lateral rotations, cross-body, sequential movements,
extensions, quick position changes, side-to-side weight
shifting)
How does exercise help brain function in
Parkinson’s?
Exercise can help increase brain volume, improving
working memory and attention. Also, it increases blood
vessels and leads to more neurotrophic (growth) factors
(like “gatorade” for the brain!) and a more supportive
environment for neurons. Exercise also increases the
redundancy in brain synapses. Redundancy is good! If you
have some synapses that aren’t working, you will have
back ups to replace them!
Specifically in PD, research tells us that exercise
increases survival rate, increases physical functional
ability, and improves cognition! It can help “repair”
the dopamine system in early/moderate stages of PD by
increasing dopamine D2 receptors and helping your brain
make better use of remaining dopamine.
Last revised: 10/17/16
by Kristine Decant, PT
References
“How might physical activity benefit patients with
Parkinson disease?” Speelman, Nature Reviews, 2011
“Effectiveness of intensive inpatient rehabilitation
treatment on disease progression in parkinsonian
patients” Giuseppe et al., Neurorehabil Neural Repair,
2012
Neurodegener Dis Manag. 2011 Apr 1;1(2):157-170.
Ahlskog JE. Neurology 2011;77:288-295.
“Does vigorous exercise have a neuroprotective effect in
Parkinson disease?” Ahlskog Je, Neurology, 2011
Farley BG, Koshland GF. Experimental Brain Research
2005;167(3):462-467.
Exp Brain Res. 2005 Dec;167(3):462-7. Epub 2005 Nov 11.
Training BIG to move faster: the application of the
speed-amplitude relation as a rehabilitation strategy
for people with Parkinson's disease.
Farley BG, Koshland GF.
Farley BG, Fox CM, Ramig LO, McFarland, D. Top Geriatric
Rehabilitation 2008;24(2):99-114.
King LA, Horak FB. Physical Therapy 2009;89:384-393.
Kleim, JA, Jones TA. Journal of Speech Language Hearing
Research 2008;51(1):S225-S239.
Petzinger GM, Fisher BE, McEwen S, Beeler JA, Walsh JP,
Jakowec M. Lancet 2013;12:716-726.
Petzinger, G, Fisher, B.E., Jacobson, S., Beeler, J.A.,
Walsh, J.P. and Jakowec, M.W. (2013). Exercise-enhanced
neuroplasticity targeting motor and cognitive circuitry
in Parkinson’s disease. Lancet Neurology, v12, pp.
716-726.
Petzinger GM, Fisher BE, Van Leeuwen JE, et al. Movement
Disorders 2010;26(Suppl 1):S141-S145.
The role of exercise in facilitating basal ganglia
function in Parkinson's disease.
Petzinger GM1, Fisher BE, Akopian G, Holschneider DP,
Wood R, Walsh JP, Lund B, Meshul C, Vuckovic M, Jakowec
MW.
Petzinger GM, Holschneider DP, Fisher BE, McEwen S,
Kintz N, Halliday M. et al. Brain Plasticity
2015;1:29-39.
The Effects of Exercise on Dopamine Neurotransmission in
Parkinson's Disease: Targeting Neuroplasticity to
Modulate Basal Ganglia Circuitry.
Petzinger GM, Holschneider DP, Fisher BE, McEwen S,
Kintz N, Halliday M, Toy W, Walsh JW, Beeler J, Jakowec
MW.
Brain Plast. 2015;1(1):29-39.
Speelman AD, van de Warrenburg BP, van Nimwegen M,
Petzinger GM, Munneke M, Bloem Br. Nature Review
Neurology 2011;7:528-534
|