The first question I often hear upon evaluation of an athlete
following an ACL repair is, “When will I return to playing
basketball/soccer/football?” The literature on when to send an
athlete back to contact sports varies from 3-12 months (1). It
becomes difficult to predict, as a clinician, on when likely return
is, secondary to the many variables such as physician preference,
the pt’s injury history, type of ACL repair, type of rehabilitation
protocol, etc. to factor into your estimation. The numerous
variables from individuality and the variance in the literature
recommendations give little guidance to clinicians. The following
article is meant to give clinicians a guide on clinical decision
making for return to sport following ACL repair.
Typically, return to full involvement in sports, according to
protocols is 6 months after surgery, and accelerated rehab programs
allow their patients to return to full sport around 4 months (1).
According to Kvist (2005), return to sport is the secondary goal,
fulfilling the criteria of the protocol for return to sport is the
primary goal.
Criteria for return to sport following ACL repair often includes
full knee AROM, resolution of pain, no joint effusion present, and
less than a 10% performance and strength deficits when compared to
uninjured knee(1). There are often other measurements as well in
literature including KT-1000 testing (anterior-posterior
translation), and isokinetic testing. Both of these require
expensive equipment that many clinics lack.
The performance aspect of the testing often uses single limb hop
testing for distance. This area of outcome testing is meant to
compare lower limbs for functional differences. Single limb hop
tests have very low sensitivity to detect abnormal limb function. In
ACL deficient knees (without repairs), 50% continue to perform
normally in single limb hop tests (2). Although scores that
demonstrate abnormality on single limb hop test are correlated with
quad weakness, and self assess difficulty of pivoting, and twisting
(2).
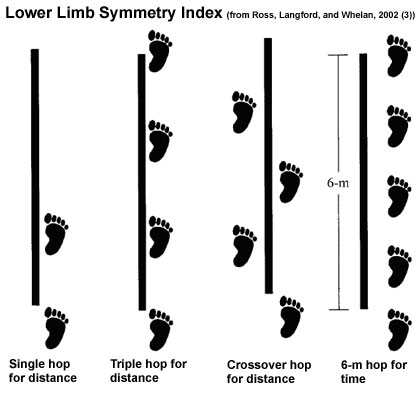
To increase testing sensitivity to abnormal function of lower
extremities, Noyes et al., recommend using a battery of tests that
they deemed as the Lower Limb Symmetry Index. This symmetry index
includes single limb hop test, timed 6m hop test, triple hop for
distance (single limb), and cross over hop for distance (see image
below). This battery of tests have increased sensitivity, with 58%
of ACL deficient knees scoring abnormally, which researchers defined
as scoring 85% or less of the unaffected leg scored(2). The authors
recommend using at least 2 of the above functional hop tests. These
tests, unlike isokinetic and KT-1000 testing require very little
equipment, space or time. Hop testing has been shown to be valid and
reliable in multiple studies for healthy and injured participants
(3,4). Note: Most ACL protocols do not allow jumping activities to
begin until 16 weeks post operatively, and clinicians should consult
either protocol or physician before performing these tests.
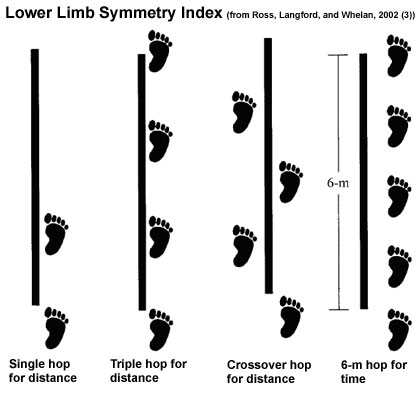 |
Calculating the Lower Extremity Symmetry Index (LSI)
A. Distance Measures: LSI = involved side/uninvolved side x
100%
B. Time Measures: LSI = uninvolved side/involved side x 100%
Hop testing incorporates sport specific requirements including
directional changes, speed, lower limb confidence, strength/control
and acceleration and deceleration (4). Despite the functional and
demanding nature of hop testing, there is very little research on
the predicative value of these tests on injury after returning to
sports, none found during the research period of this article. There
is however, a test that does have support for its predictive value
for injury after returning to sport after lower extremity injury.
This test is the Star Excursion Balance Test (5,6). A panel at
Cincinnati Children’s Hospital Medical Center recommended to add the
Star Excursion Balance Test to a functional test battery for return
to sport following lower extremity injury.
The original study reported
that those with composite reach distance scores of less than 94% of
their limb length were significantly more likely to sustain a lower
extremity injury during the athletic season
(6). The Star Excursion Balance Test had participants stand
on 1 leg and reach with opposite limb in 3 directions including,
anterior, posteromedial, and posterolateral. Composite scores summed
the reaches in all the directions and divided by the patient’s leg
length (6).
Calculating the Star Excursion Balance Test (SEBT)
SEBT = ((Ant. Distance + Post. Lat. Distance + Post. Med.
Distance)/Leg Length of Stance Limb) x 100%
In conclusion, the use of a battery of functional tests following
ACL repair would be best to determine readiness to return to sport
and reduce risk of injury upon return to sport. Research supports
the use of the Lower Limb Symmetry Index (4 part hop test), and the
Star Excursion Balance Test because they are practical, valid,
reliable and mimic the requirements of sports. Requirements for
these tests, for return to sport, include 85% or more on the LSI,
and at least 94% of limb length on the SEBT (2,4,5,6). Patients
following this surgical repair must also meet the other requirements
of their protocol, likely including full range of motion, resolution
of pain and 90% strength of their uninjured limb for safest return
to sport. Physician clearance is also recommended. So, when your
next patient following ACL repair asks you when they will return to
sport, tell them, “When you can demonstrate you are ready.”
Last revised: September 11, 20111
by Amber Wacek, DPT
References:
1. Kvist, J. Rehabilitation following anterior cruciate
ligament injury. Sport Med. 2004;34(4):269-280.
2. Noyes, F.R. et al. Abnormal lower limb symmetry determined by functional
hop test after anterior cruciate ligament rupture. Am J Sport Med.
2004;19(5):513-518.
3. Ross, M.D., Lanford, B., & Whelan, P. Test-retest reliability of 4
single-leg horizontal hop tests. Journal of Strength & Conditioning.
2002;16(4): 617-622.
4. Reid, A., Birmingham, T.B., Stratford, P.W., Alcock, G.K., & Giffin, J.R.
Hop Testing provides a reliable and valid outcome measure during
rehabilitation after anterior cruciate ligament reconstruction. Physical
Therapy. 2007;87(3):337-349.
5. Cincinnati Children’s Hospital Medical Center Return to Activity
Evidence-Based Practice Team 2009. Evidence Based Care Guideline for Return
to Activity after Lower Extremity Injury. (2010) p. 1-13. Guideline 38.
6. Plisky, P.J., Rauth, M.J., Kaminski, T.W., & Underwood, F.B. Star
Excursion Balance Test as a predictor of lower extremity injury in high
school basketball players. J Orthop Sports Phys Ther. 2006;36(12): 911-919.