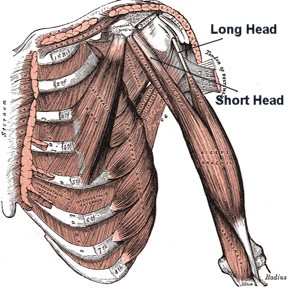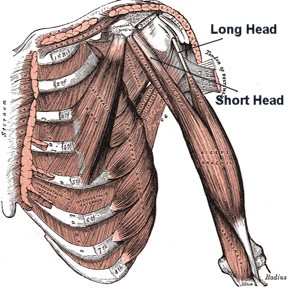
The biceps brachii muscle is a two-headed muscle responsible for
flexing the elbow and supinating the forearm (1). The long head
originates on the supraglenoid tubercle of the scapula and
courses through the bicipital groove under the transverse
humeral ligament (1). The short head originates on the coracoid
process of the scapula (1). Both heads join near the insertion
of the deltoid to form a common muscle belly (1,2). Distally,
the muscle belly splits into two tendons with the stronger
tendon attaching to the radial tuberosity and the other tendon
attaching to the fascia of the forearm via the bicipital
aponeurosis (1,2).
Biceps tendinitis vs. biceps tendinosis
The phrase tendinitis implies inflammation, while the phrase
tendinosis implies collagen degeneration (3). Chronic tendinitis
may require 4-6 weeks to completely heal, while chronic
tendinosis may require 3-6 months for full recovery (3).
According to an article by Khan et al., an increasing body of
evidence supports that many overuse tendon injuries do not
involve inflammation (3). Therefore, these tendon injuries
should be labeled overuse tendinosis instead of overuse
tendinitis.
Supporting the rarity of tendinitis discussed in the
aforementioned Khan et al. article, Churgay estimates that
approximately 5% of patients with proximal bicep tendon injuries
suffer from primary biceps tendinitis, or inflammation of the
biceps tendon within the bicipital groove (4). Overhead and
repetitive shoulder rotation activities worsen the tendinitis,
causing the tendon to degenerate, thicken, and become irregular
(4). This collagen disorientation and disorganization is a
histologic trademark of tendinosis (3). Churgay notes that
athletes over age 35 or nonathletes are more likely to have
biceps tendinosis as a result of overuse over time (4). Primary
impingement, which occurs via mechanical compression of the
rotator cuff, biceps long head, and subacromial bursa between
the humeral head and the acromion, is considered the most common
cause of biceps tendinosis (5,4).
Subjective Exam
Patients may complain of sharp pain in the front of the shoulder
when reaching overhead, pain that radiates toward the neck or
down the front of the arm, dull achy pain at the front of the
shoulder after activity, and difficulty with daily activities
such as putting dishes away in overhead cabinets (6). Patients
with secondary impingement, which is a relative decrease in the
subacromial space with excessive anterior and superior migration
of the humeral head caused by instability in the glenohumeral
joint, may complain of numbness and tingling into the arm, pain
in the anterior/lateral shoulder, and pain in surrounding
musculature (5).
Objective Exam
The most common finding of proximal biceps tendon injury is
bicipital groove point tenderness (4). Many special tests,
including Yergason, Neer, Hawkins, and Speed, are useful in
implicating pathology of the biceps tendon (4). However, since
these tests also create impingement under the coracoacromial
arch, it is important to note that a rotator cuff lesion may
also elicit pain and contribute to a positive test result (4).
Conservative Treatment
Conservative treatment consists of rest from overhead activity
and ice (20 minutes at a time several times a day) (7). A doctor
may also recommend NSAIDs to reduce pain and swelling,
corticosteroid injections, and physical therapy (7).
Physical therapy management of proximal biceps tendon injuries
typically consists of three phases: phase one (restoration of
full PROM, pain management, and restoration of normal accessory
motion), phase two (AROM exercises and early strengthening), and
phase three (rotator cuff and periscapular strength training,
with a focus on enhancing dynamic stability) (2). For athletes,
a return to sport phase is initiated upon completion of the
rotator cuff and periscapular strength training phase (2).
Advancement through the phases depends on the chronicity and
irritability of the injury. A physical therapist will be best
able to guide patients through the proper exercise progression
based on pain, swelling, and motion. The American Academy of
Orthopaedic Surgeons has created a detailed handout that
clinicians and patients alike may find helpful titled "Shoulder
and Rotator Cuff Exercise Conditioning Program" (8). This
handout is available online at:
http://orthoinfo.aaos.org/PDFs/Rehab_Shoulder_5.pdf
Surgical Management
If a patient fails three months of conservative treatment,
surgery may be considered (4). During surgery, structures
causing impingement may be removed and the tendon may be
debrided (4). For serious tears or complete ruptures of the
biceps long head tendon, a biceps tenodesis may be performed
(4). This operation involves attaching the cut biceps tendon to
the bicipital groove or transverse humeral ligament with sutures
or anchors (4). A biceps tenotomy may also be performed (4).
This operation involves removal of the ruptured biceps tendon
from the glenohumeral joint and is "the procedure of choice" for
inactive patients over the age of 60 with a completely ruptured
biceps tendon (4).